Taste Alterations: Clinicians’ Perspective on Cancer Patient Outcomes and Management Strategies
Lakmani T. Galaniha and Alissa A. Nolden*
Department of Food Science, University of Massachusetts, Amherst, MA 01003, United States
Abstract
Taste alterations, a common treatment-related side effect among cancer patients, with up to 93% complaining of taste-related symptoms. Even with its high prevalence, patients report a lack in support from clinicians. Clinicians’ perspective regarding taste alterations among cancer patients is not well understood. Thus, this study examines clinicians’ perspectives regarding taste alterations among cancer patients. In an online survey, sixty-seven clinicians practicing in the United States and working with cancer patients complaining of taste problems answered questions on their experience treating patients' taste alteration symptoms.
Clinicians are most concerned about the impact of taste alterations on nutritional intake, emotional distress, and overall quality of life. 73% reported understanding the patient's taste alterations was important or very important. Yet roughly 75% thought it was challenging to recommend strategies to manage their symptoms, and nearly all reported feeling frustrated when supporting patients’ taste alterations. Regarding management strategies, clinicians mostly suggested dietary counseling, drinking plenty of fluids during meals, and changing the texture of the food, with some success reported for these strategies. This study provides new insight into clinicians’ experiences supporting cancer patients with taste alterations, helping identify knowledge gaps. A lack of evidence-based taste management strategies poses a significant challenge for clinicians in managing patients' taste alterations. These results emphasize the need to develop education and training material and identify effective treatment strategies to assist clinicians in providing better-quality care for patients suffering from taste alterations.
Introduction
Cancer treatments cause many unpleasant side effects, including taste alterations, which is one of the most common complaints among cancer patients, with prevalence rates estimated between 17.6 – 93% 1–6. Altered taste perception is often accompanied with other treatment-related side-effects impacting the gastrointestinal system, with high co-occurrence rates reported for loss of appetite7, oral problems including dry mouth2,7,8 and other food-related problems including food aversions and malnutrition9–11. Changes in taste or altered taste perception can result in a decline in cancer patients' overall quality of life due to its impacts on physical and psychosocial dimensions2–5,7,12–15.
Current data suggests that taste alterations arise in cancer patients during and after cancer treatment. Chemotherapy and radiation therapy are known to damage taste cell renewal, reduce the number of taste cells within taste buds, and are associated with changes in the expression of taste receptors in the oral cavity 16–18. Despite the impact of taste alterations on food behaviour19, nutritional status, and quality of life2,20,21, it has been reported that cancer patients mostly try to deal with their taste alteration management independently with limited support from health care professionals.
While taste loss or changes in taste are common phrases used to describe taste alterations among cancer patients, these symptoms are classified as a taste disorder, with dysgeusia being the clinical classification. There are several different sub-types of taste disorders, many of which have been reported by cancer patients, including a reduction in taste sensitivity (hypogeusia), enhancement of taste sensitivity (hypergusia), complete loss of taste sensitivity (ageusia), persistent perception of unpleasant sensations such as bitterness or metallic sensation (pallinageusia), or perception of a taste in the absence of a stimulus (phantageusia) 6,12,22–24. One challenging aspect of using these terms is that patients’ self-report of these symptoms are often diagnosed as dysgeusia without psychophysical assessment; therefore, it is difficult to estimate the number of patients experiencing different classifications of taste disorders. Hence, details about patients’ severity and pattern of the occurrence of taste alterations are still lacking a common agreement 25, and could be a primary reason for the gap in the available treatments and coping strategies for taste alterations.
In addition to a lack of empirical studies examining management strategies for taste alteration, patients have reported receiving inadequate support from clinicians 13. In a qualitative study of lung cancer patients, Belqaid and colleagues (2018) reported that cancer patients suffering from taste alterations relied on self-driven support or family/community-based resources for coping mechanisms and adjusting their lives to live with taste changes without clinicians' support 13. This lack of support and adjustment to daily life negatively impacts the quality of life. It interferes with daily activities and social rituals around dining events and reports disappointment, frustration, and sadness13,15,26,27. Some patient- and caregiver-driven strategies have been found to help improve nutrition and food liking through carefully designed recipes 28–30. There is currently a gap in understanding the clinician’s perspective, specifically how they engage with patients regarding symptoms of taste loss. Some prior studies suggest that clinicians may consider taste alterations non-life-threatening, and a lack of proven taste management strategies has limited their involvement 4,13,31. To address this knowledge gap, we conducted an online survey to examine clinicians’ perspectives and concerns about taste alterations in cancer patients and their knowledge of taste alteration management strategies. This information will help establish clinicians' understanding of taste alterations and identify opportunities to implement taste management strategies reported to improve patients' taste alteration symptoms.
Methods
Study Participants
For this study, we recruited clinicians working with cancer patients complaining of taste problems. Potential clinicians were targeted using social media networking websites and professional networks, as well as posting advertisements in hospitals. The eligibility criteria included being at least 18 years old, residing in the U.S., and working with cancer patients who complain of taste problems. The survey was accessible between January 2020 through February 2021 and was hosted on Compusense Cloud software (Guelf, Canada). The online survey was approved by The Institutional Review Board at The University of Massachusetts.
Questionnaire
Clinicians provided informed consent prior to accessing the survey. The survey included questions related to demographic information, including age, gender, and ethnicity, as well as questions related to profession and professional experience, including the number of years in practice and the cancer types of the patients they work with. The present analysis investigated questions related to their perspective and concerns about taste alterations when treating cancer patients and their knowledge of management strategies for taste alterations (Figure 1).
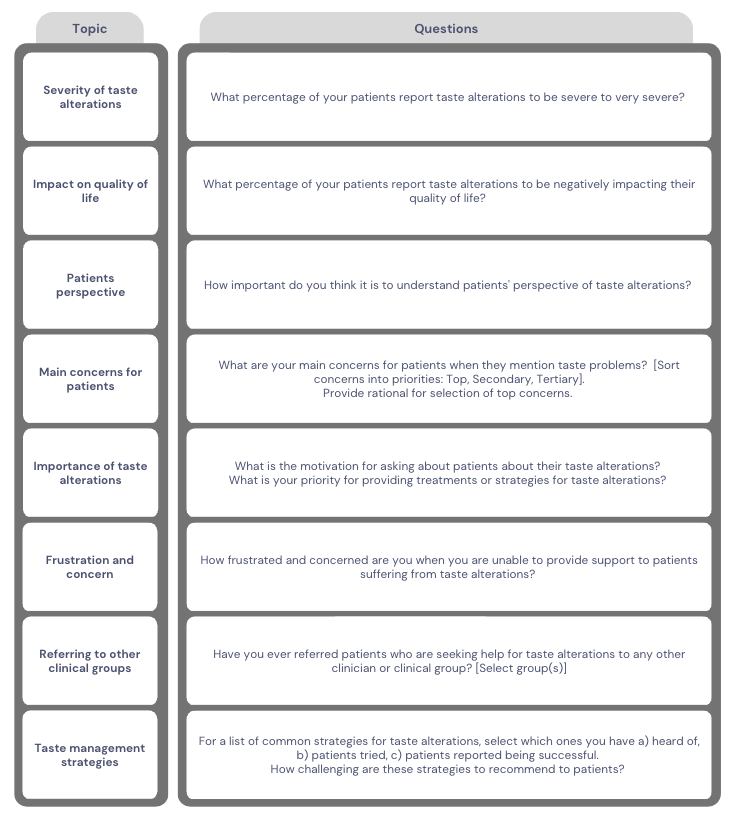
Figure 1: Questions assessing clinicians’ perspective and concerns of taste alterations in cancer patients and their knowledge on taste alteration management strategies.
Statistical Analysis
Clinicians’ responses were analyzed by performing descriptive statistics using R Studio (version 3.6.2). NVivo 12 Plus (version 12.6.0) was used to analyze themes for coded open-ended questions.
Results
Participant Characteristics
Among the total of 76 consented clinicians, 71 completed the survey questionnaire. Four clinicians who indicated that they were not working with patients complaining of taste problems were removed from the survey as they were ineligible to participate per the inclusion criteria. The final analysis consists of data from 67 clinicians, among which the majority were females (74.6%) and White (74.6%) in the age category 25-34 years old (58.2%). Most of the clinicians reported having less than 10 years of professional experience (61.2%), and most clinicians were otolaryngologists (34.3%) and speech pathologists (28.4%). The demographic information of the clinicians has been summarized in Table 1.
Table 1: Demographic information of clinicians
|
|
|
n |
% |
|
Gender
|
Female Male |
50 17 |
74.6 25.4 |
|
Age (years)
|
25 – 34 35 – 44 45 – 54 55 – 64 > 64
|
39 14 2 7 5 |
58.2 20.9 3.0 10.5 7.5 |
|
Ethnicity
|
Asian Black or African American Hispanic or Latino White Mixed Race
|
10 1 2 4 50 4 |
15.0 1.5 3.0 6.0 74.6 6.0
|
|
Profession
|
Dietitian Nurse Oncologist Otolaryngologist Speech Pathologist Other |
8 5 2 10 23 19 |
11.9 7.5 3.0 34.3 28.4 14.9 |
|
Years practicing |
1-10 11-20 21-30 31-40 41-50
|
41 15 3 7 1 |
61.2 22.4 4.5 10.4 1.5
|
Clinicians’ perspective of taste alterations
The majority of clinicians (44%) indicated that understanding patients’ perspective of taste alterations to be ‘very important’ (Figure 2). Roughly a quarter of clinicians (25%) indicated it is fairly or slightly important to understand patients’ perspectives of taste alterations.
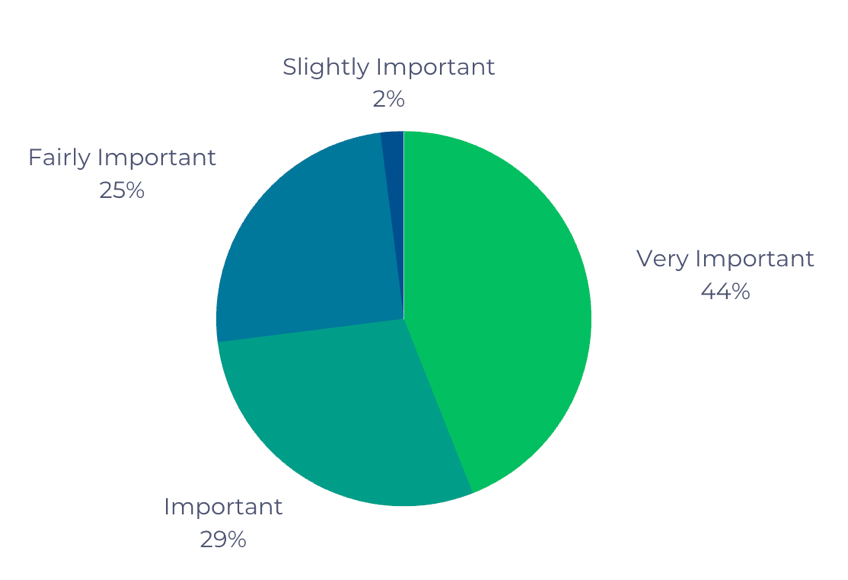
Figure 2: The importance of understanding patients’ perspective of taste alterations.
The clinicians were asked about their main concerns regarding their patients’ complaints about taste alteration. To identify the top taste-related concerns, clinicians were asked to categorize six symptoms (i.e., Oral health status, GI symptoms, Impact on appetite and food intake, Impact on quality of life, Impact on emotional distress, and ‘other’) as either a top, secondary, or tertiary concern, with a max of three symptoms to each category. It was not a requirement to select all the symptoms. The symptoms selected as a top concern were ‘impact on appetite and food intake’ and ‘emotional distress,’ both selected by 82% of clinicians. The most commonly selected symptom categorized as a secondary concern was the impact on quality of life (52.5%), and the tertiary concern was oral health (32.8%). Results of this task are reported in Table 2, displaying the percentage of clinicians' selection of symptoms as top, secondary, and tertiary concerns.
Table 2: Percent of clinicians categorization of taste-related symptoms as either top, secondary, or tertiary concern.
|
|
Top (%) |
Secondary (%) |
Tertiary (%) |
|
Impact on appetite and food intake |
82.0
|
14.8
|
3.3
|
|
Impact on emotional distress |
82.0 |
14.8
|
3.3
|
|
Oral health |
36.4
|
31.8
|
31.8
|
|
Impact on QOL |
29.5
|
52.5
|
18.0
|
|
GI symptoms |
24.1
|
51.7
|
24.1
|
|
Other concerns |
9.1
|
0.0 |
90.9
|
Once the clinicians selected the top concerns, they were asked to provide a rationale for the symptoms selected. Clinicians described the challenge in maintaining weight, the impact on oral food intake and swallowing functions, the impact on nutritional and hydration status, and social isolation.
Motivation to Support Patients with Taste Alterations
Prior research suggests clinicians may not prioritize patients' taste alteration symptoms as it is not life-threatening 32. To better understand clinicians' motivation to support cancer patients experiencing taste alterations, we asked clinicians the reasons for asking their patients about their taste alterations by selecting: “Guide treatments/intervention plan,” “Improve quality of life,” or “Other.” The top selected answer was to improve their quality of life (61%), followed by guiding treatment plans (50.9%). Clinicians were then asked to rank their priority for managing taste alteration symptoms as either low, medium, high, urgent priority, or no priority (see Figure 3). Most clinicians (69%) reported that managing taste alterations was a medium priority, followed by high priority (18.2%) and low priority (12.7%). None of the clinicians indicated that managing taste alterations was an “urgent” priority.
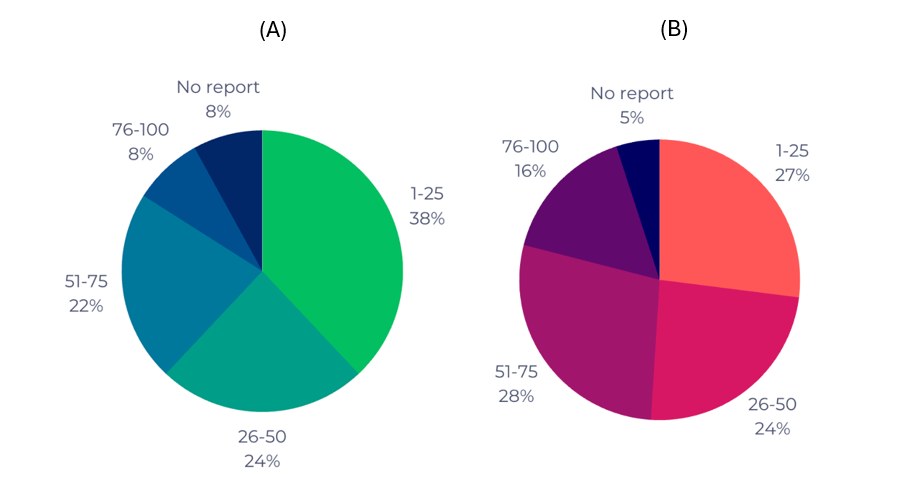
Figure 3: Percentage of clinicians who indicated the percentage (range) of their patients describing A) taste alterations to be severe to very severe and B) taste alterations to impact quality of life.
Clinicians Experiences with Taste Alterations in Cancer Patients
Clinicians answered several questions directed at understanding their perception of cancer patients' experiences with taste alterations. Regarding the perceived patient severity of taste alterations, we asked clinicians to select a percentage range of patients that described their taste alterations as severe to very severe (Figure 3A). The most commonly selected response was 1-25% of patients (38%), followed by 26-50% (24%) and 51-75% (22%), with fewer clinicians selecting 76-100% (8%). However, 8% of clinicians indicated that their patients do not report the severity of their taste alterations.
Next, the clinicians were asked to report the percentage (range) of their patients who discuss or communicate the impact of taste alterations on the quality of life (Figure 3B). The highest selected percentage range, with 28% of clinicians reporting that 51-75% of their patients report taste alterations impacting quality of life. Another quarter of participants each selected 1-25 and 26-50 percent of patients (27% and 25%, respectively). While 16% reported that 76-100% of patients reported the impact of taste alterations on quality of life, 5% reported that patients did not report the impact on quality of life.
Clinicians' Experiences with Providing Support and Management Strategies for Taste Alterations
A series of questions aimed to capture clinicians' experiences and knowledge of supporting and management strategies for taste alterations. Often, clinicians may refer to a specialist or another clinician group to support their patients. Here, we asked clinicians to select the clinician group or other specialist that cancer patients may be referred to for receiving support for taste alterations. The most common clinician group selected was Dentists (21.8%), followed by otolaryngologists (12.7%), with 18.2% reporting that they refer to ‘other’ clinicians. The specifications for ‘other’ types of clinicians included Dietitians, Nutrition Counselors, Acupuncturists, and Smell and Taste Center.
Many management strategies in the literature or posted on cancer support groups (e.g., American Cancer Society) may be helpful for patients experiencing taste alterations. However, most of these have yet to be clinically evaluated, except for zinc supplementation, which has conflicting results in clinical trials 31. To better understand clinicians’ experiences and perceptions of these management strategies, clinicians were asked about their experiences with patients regarding taste management strategies. Clinicians were shown a list of taste management strategies identified in the literature and through cancer support websites. Clinicians were asked to select all the strategies (i.e., “check all that apply”) for each of the following conditions: i) if they have heard about the strategy, ii) if they know if their patients have tried it, and iii) whether patients found it to be successful (see Table 3). The majority of the clinicians reported dietary counseling, drinking plenty of fluids during the meal, changing the texture of the food, oral care before eating, and chewing the food slowly and thoroughly as strategies they have heard of and found patients to report them to be successful at managing taste alterations. Adding food additives was not reported by clinicians to be a commonly heard about strategy but was just as effective at managing taste alterations as chewing food slowly.
Table 3: Percent of clinicians reporting on taste management strategies
|
Taste management strategies |
Clinicians have heard%(n) |
Patients have tried %(n) |
Patients found successful %(n) |
|
Dietary counselling |
69.1(38) |
58.2(32) |
29.1(16) |
|
Drink plenty of fluids during the meal |
67.3(37) |
61.8(34) |
30.9(17) |
|
Change texture of the food |
58.2(32) |
54.6(30) |
29.1(16) |
|
Oral care before eating |
52.7(29) |
47.3(26) |
32.7(18) |
|
Chew the food slowly and thoroughly |
50.9(28) |
56.4(31) |
27.3(15) |
|
Food additives (e.g., Spices) |
38.2(21) |
34.6(19) |
27.3(15) |
|
Sialagogues |
38.2(21) |
34.6(19) |
18.2(10) |
|
Take pain medication before eating |
38.2(21) |
30.9(17) |
18.2(10) |
|
Medications that included cannabinoid dronabinol |
38.2(21) |
23.6(13) |
20.0(11) |
|
Switch between food during meal |
34.6(19) |
34.6(19) |
14.6(8) |
|
Mindfulness and mindful eating |
34.6(19) |
23.6(13) |
18.2(10) |
|
Zinc supplements |
25.4(14)
|
10.9(6) |
3.6(2) |
|
Acupuncture |
20.0(11) |
10.9(6) |
9.1(5) |
|
Avoid the environment where the food is being cooked |
20.0(11) |
10.9(6) |
5.5(3) |
|
Miracle berry tablets |
18.2(10) |
9.1(5) |
5.5(3) |
|
Medications that included megestrol acetate |
16.4(9) |
14.6(8) |
7.3(4) |
|
Herbal medicine |
10.9(6) |
7.3(4) |
1.8(1) |
|
Liposomal nose and mouth spray |
10.9(6) |
5.5(3) |
1.8(1) |
|
Medications that included clonazepam |
10.9(6) |
1.8(1) |
0.0 |
|
Supplement with vitamin D |
7.3(4) |
5.5(3) |
0.0 |
|
Refer to a specialized institute |
5.5(3) |
3.6(2) |
3.6(2) |
|
Other |
5.5(3) |
0.0 |
1.8(1) |
|
None of the above* |
3.6(2) |
7.3(4) |
18.2(10) |
*None of the above indicates that none of the strategies listed above was heard, tried, or found to be successful.
Clinicians were asked how challenging it is to prescribe or suggest these strategies to their patients (a little bit, somewhat, quite a bit, very much). Somewhat, a little bit, and quite a bit were reported by 50.9%, 18.2%, and 14.6% clinicians, respectively. Only 7.3% reported it as ‘very much ‘challenging, yet 9.1% reported it as ‘not at all’ challenging.
When the clinicians were asked how frustrated or concerned they are when they are unable to provide support to patients suffering from taste alterations as clinical professionals, the majority (44%) reported being somewhat frustrated, 32% reported being quite a bit frustrated, 16% reported to be very much frustrated, while 8% reported to be a little bit frustrated.
Discussion
The current study explored clinicians' perspectives and concerns regarding taste alterations and management strategies. This is the first empirical investigation to assess the clinicians’ perspective regarding supporting and managing cancer patients’ taste alterations. The current study provided an in-depth understanding of the perspective of healthcare professionals about taste alteration in cancer patients and the challenges they face when helping cancer patients with their taste management. We report new evidence contrary to prior studies suggesting clinicians do not prioritize changes in taste function; rather, clinicians are reporting taste alterations as an essential symptom tied to appetite and food intake, emotional distress, gastrointestinal symptoms, and quality of life. Clinicians report feeling very frustrated when they cannot support their patients' taste alterations and report it is challenging to suggest management strategies.
Prior work suggests that patients are not getting adequate support from clinicians, with patients seeking support from other resources such as family members and social and community networks 13. There is an opportunity for clinicians to play a more supportive role in helping patients manage their taste alterations. To improve the engagement between patient and clinician, more information is needed from the clinicians’ perspective regarding their experience with taste alterations. Together, this information provides important insight for targeting opportunities for improving knowledge, resources, and tools to equip clinicians better to support their patients.
Clinicians reported taste alterations impacting appetite, food intake, and emotional distress. Other studies have reported that changes in taste function can have adverse health outcomes, including reduced appetite, weight loss, and quality of life. Patients with severe chemosensory-related complaints (e.g., bad taste in the mouth, taste distortion) reported consuming significantly fewer calories, having higher rates of weight loss, and having lower quality of life than patients with mild or moderate chemosensory complaints20. Changes in taste function, taste alterations, and other taste disorders are repeatedly associated with loss of appetite, weight loss, gastrointestinal symptoms, and quality of life 9–11,33–36. The reduction in oral food intake may lead to the disuse atrophy of the swallowing muscles, which could impact the swallowing functions in patients 37. It also directly affects a patient's nutritional and hydration status, causing them poor treatment outcomes38,39. Our study demonstrates that clinicians are aware of the importance and implications of taste alterations on the overall health of their patients. However, there remain challenges when offering support to patients to help manage taste alterations.
The present study revealed that almost half of the clinicians found themselves quite a bit frustrated or concerned about not being able to their patients suffering from taste alterations. These findings emphasize clinicians' concerns for cancer patients suffering from taste alterations. Whereas previous studies suggest lack of attention to chemosensory complaints is due to the symptom not being life-threatening 32, this may not be accurate. Instead, the lack of support may be due to other challenges, such as inadequate access to educational materials and training on taste alterations40 and treatment or management options 13. In response, it has been suggested that healthcare professionals are in a position to recommend patients experiment with strategies on their own 13,38. However, there is still a lot of uncertainty around the recommended taste management strategies. Recent studies suggest that patient and caregiver-initiated strategies for living with taste changes can improve flavor of food through modifying meal preparation and recipies based on the patients’ altered taste function. In other words, caregivers work with patients to identify what sensations they can still perceive and enjoy and adapt recipes to make food more flavorful and enjoyable28–30. These approaches can be encouraged by clinicians but it can take time through trial and error to try new recipes41. While these approaches are promising strategies for patients to adapt their lives to taste changes, more work is needed to determine if this can be a long-term solution and whether this has any improvement on nutritional status. As pointed out in several recent reviews, there is conflicting or a lack of evidence for effective treatment or management strategies for taste disorders42–44.
This study provides important new insights regarding clinicians’ experiences with common taste management strategies. Taste management strategies were found in the literature13,45,46 and from publicly available cancer patient support websites. Clinicians reported being most familiar with “oral care before eating” and “drinking plenty of fluid during meals,” which were thought to be the most successful taste management strategies. Oral care and oral health are essential symptoms for many cancers 1,46 and recommended to see a dentist regarding managing oral health symptoms 46. Changes in taste and taste disorders have been linked with changes in saliva production, dry mouth, and xerostomia 47. Drinking more fluids may help to improve salivary flow rate and dry mouth symptoms. Thus, this strategy may improve taste function 47. Further, it’s been reported that doing oral evaluations before beginning cancer treatments could identify oral infections, fractured teeth or restorations, and periodontal diseases, which could contribute to oral complications upon cancer therapy. Yet, there is a lack of empirical evidence demonstrating that oral care before meals or drinking more fluids effectively managed taste alterations. These strategies should be evaluated to determine their effectiveness, including testing a combination of strategies and the need to consider demographic or clinical characteristics (e.g., chemotherapy drug or type of taste disorder).
This data provides a small glimpse into potential strategies that may be effective, yet out of the 21 potential strategies, only 5 strategies were familiar to half of the clinicians. This demonstrates that clinicians need to be made aware of most strategies, with even fewer reported as being effective for their patients. Boltong and colleagues noted that the lack of evidence-based practice in taste management strategies causes healthcare professionals to feel uncertain when suggesting taste management strategies to their patients45. This agrees with the present study, with clinicians reporting it challenging to recommend treatment options to their patients. Empirical evidence through clinical trials is urgently needed to identify management strategies for taste alterations. Translational research, bringing together researchers and clinicians, is essential for identifying effective treatments for managing taste alterations, which could profoundly impact clinicians and their patients. Our study revealed that patients may be referred to dentists, otolaryngologists, dietitians, acupuncturists, oncology doctors, nurses, and palliative home care teams are the most known clinical professionals 13,45. This comprehensive team of clinicians can bring together unique perspectives and considerations, helping to increase the successful identification of effective treatment strategies.
Conclusion
The present study highlights the clinicians’ perspective on treating cancer patients with taste alterations and their experiences with management strategies for taste alteration symptoms. Clinicians are motivated to identify taste alteration management strategies for cancer patients to improve nutritional intake, reduce emotional distress, and enhance patients' overall quality of life. Managing patients’ taste alterations is a medium priority (below a high or urgent priority). This work emphasizes the need to implement evidence-based taste management strategies to prepare healthcare professionals to better care for cancer patients suffering from taste alterations. Further, evidence-based strategies for managing taste alterations should be identified, which may help to increase clinicians’ confidence in suggesting and treating patients’ taste symptoms. Clinicians equipped with successful taste management strategies would positively change cancer patients' nutritional intake, emotional distress, and quality of life.
Disclosures and Acknowledgments
Acknowledgments: None to report.
Funding: LTG is funded by the UMass Amherst and Salmon Fellowship (U103576000000A).
Conflict of interest statement: The authors have no conflicts of interest to declare.
During this work, Dr. Nolden received research support (unrelated to this study) from the National Institutes of Health.
References
- Larsen AK, Thomsen C, Sanden M, et al. Taste alterations and oral discomfort in patients receiving chemotherapy. Supportive Care in Cancer. 2021; 29(12): 7431-7439. doi: 10.1007/s00520-021-06316-4.
- Gamper EM, Giesinger JM, Oberguggenberger A, et al. Taste alterations in breast and gynaecological cancer patients receiving chemotherapy: Prevalence, course of severity, and quality of life correlates. Acta Oncol (Madr). 2012; 51(4): 490-496. doi: 10.3109/0284186X.2011.633554.
- Gwede CK, Small BJ, Munster PN, et al. Exploring the differential experience of breast cancer treatment-related symptoms: A cluster analytic approach. Supportive Care in Cancer. 2008; 16(8): 925-933. doi: 10.1007/s00520-007-0364-2.
- Zabernigg A, Gamper E, Giesinger JM, et al. Taste Alterations in Cancer Patients Receiving Chemotherapy: A Neglected Side Effect? Oncologist. 2010; 15(8): 913-920. doi: 10.1634/theoncologist.2009-0333.
- Bernhardson BM, Tishelman C, Rutqvist LE. Self-reported taste and smell changes during cancer chemotherapy. Supportive Care in Cancer. 2008; 16(3): 275-283. doi: 10.1007/s00520-007-0319-7.
- Hovan AJ, Williams PM, Stevenson-Moore P, et al. A systematic review of dysgeusia induced by cancer therapies. Supportive Care in Cancer. 2010; 18(8): 1081-1087. doi: 10.1007/s00520-010-0902-1.
- Nolden A, Joseph PV, Kober KM, et al. Co-occurring Gastrointestinal Symptoms Are Associated With Taste Changes in Oncology Patients Receiving Chemotherapy. J Pain Symptom Manage. 2019; 58(5): 756-765. doi: 10.1016/j.jpainsymman.2019.07.016.
- Venkatasalu MR, Murang ZR, Ramasamy DTR, et al. Oral health problems among palliative and terminally ill patients: An integrated systematic review. BMC Oral Health. 2020; 20(1). doi: 10.1186/s12903-020-01075-w.
- Muscaritoli M, Lucia S, Farcomeni A, et al. Prevalence of Malnutrition in Patients at First Medical Oncology Visit: The PreMiO Study.; 2017. www.impactjournals.com/oncotarget.
- Rahemtulla Z, Baldwin C, Spiro A, et al. The palatability of milk-based and non-milk-based nutritional supplements in gastrointestinal cancer and the effect of chemotherapy. Clinical Nutrition. 2005; 24(6): 1029-1037. doi: 10.1016/j.clnu.2005.08.003.
- Shragge JE, Wismer WV, Olson KL, et al. The management of anorexia by patients with advanced cancer: A critical review of the literature. Palliat Med. 2006; 20(6): 623-629. doi: 10.1177/0269216306070322.
- Baharvand M, Shoalehsaadi N, Barakian R, et al. Taste alteration and impact on quality of life after head and neck radiotherapy. Journal of Oral Pathology and Medicine. 2013; 42(1): 106-112. doi: 10.1111/j.1600-0714.2012.01200.x.
- Belqaid K, Tishelman C, Orrevall Y, et al. Dealing with taste and smell alterations—A qualitative interview study of people treated for lung cancer. PLoS One. 2018; 13(1). doi: 10.1371/journal.pone.0191117.
- Bernhardson BM, Tishelman C, Rutqvist LE. Taste and Smell Changes in Patients Receiving Cancer Chemotherapy Distress, Impact on Daily Life, and Self-Care Strategies.; 2009.
- Boltong A, Keast R, Aranda S. Experiences and consequences of altered taste, flavour and food hedonics during chemotherapy treatment. Supportive Care in Cancer. 2012; 20(11): 2765-2774. doi: 10.1007/s00520-012-1398-7.
- Gaillard D, Shechtman LA, Millar SE, et al. Fractionated head and neck irradiation impacts taste progenitors, differentiated taste cells, and Wnt/β-catenin signaling in adult mice. Sci Rep. 2019; 9(1): 17934. doi: 10.1038/s41598-019-54216-9.
- Jewkes BC, Barlow LA, Delay ER. Effect of radiation on sucrose detection thresholds of mice. Chem Senses. 2018; 43(1). doi: 10.1093/chemse/bjx066.
- Wang T, Glendinning J, Grushka M, et al. Drug-induced taste disorders in clinical practice and preclinical safety evaluation. Toxicological Sciences. 2017; 156(2): 315-324. doi: 10.1093/toxsci/kfw263.
- Nolden AA, Hwang LD, Boltong A, et al. Chemosensory Changes from Cancer Treatment and Their Effects on Patients’ Food Behavior: A Scoping Review.; 2019.
- Hutton JL, Baracos VE, Wismer WV. Chemosensory Dysfunction Is a Primary Factor in the Evolution of Declining Nutritional Status and Quality of Life in Patients With Advanced Cancer. J Pain Symptom Manage. 2007; 33(2): 156-165. doi: 10.1016/j.jpainsymman.2006.07.017.
- Alvarez-Camacho M, Gonella S, Ghosh S, et al. The impact of taste and smell alterations on quality of life in head and neck cancer patients. Quality of Life Research. 2016; 25(6): 1495-1504. doi: 10.1007/s11136-015-1185-2.
- Comeau TB, Epstein JB, Migas C. Taste and smell dysfunction in patients receiving chemotherapy: A review of current knowledge. Supportive Care in Cancer. 2001; 9(8): 575-580. doi: 10.1007/s005200100279.
- Leopold D. Distortion of Olfactory Perception: Diagnosis and Treatment.; 2002.
- Hirsch AR. Neurological Malingering. Taylor & Francis Group; 2018.
- Yamashita H, Nakagawa K, Nakamura N, et al. Relation between acute and late irradiation impairment of four basic tastes and irradiated tongue volume in patients with head-and-neck cancer. Int J Radiat Oncol Biol Phys. 2006; 66(5): 1422-1429. doi: 10.1016/j.ijrobp.2006.08.037.
- de Vries YC, Helmich E, Karsten MDA, et al. The impact of chemosensory and food-related changes in patients with advanced oesophagogastric cancer treated with capecitabine and oxaliplatin: a qualitative study. Supportive Care in Cancer. 2016; 24(7): 3119-3126. doi: 10.1007/s00520-016-3128-z.
- Bernhardson BM, Tishelman C, Rutqvist LE. Chemosensory Changes Experienced by Patients Undergoing Cancer Chemotherapy: A Qualitative Interview Study. J Pain Symptom Manage. 2007; 34(4): 403-412. doi: 10.1016/j.jpainsymman.2006.12.010.
- Corremans M, Verroeye A, Van Den Wijngaert L, et al. Selective Taste Management: A Selfcare Intervention for Cancer Outpatients Suffering Chemotherapy-Induced Dysgeusia Article Information. Vol 4.; 2021.
- Pritlove C, Capone G, Kita H, et al. Cooking for vitality: Pilot study of an innovative culinary nutrition intervention for cancer-related fatigue in cancer survivors. Nutrients. 2020; 12(9): 1-21. doi: 10.3390/nu12092760.
- Geurden B, Corremans M, Van den Wijngaert L, et al. Chef-led taste centers provide an accurate and integrated transmural approach to chemotherapy-induced dysgeusia in adult cancer outpatients. Int J Integr Care. 2023; 23(S1): 485. doi: 10.5334/ijic.icic23524.
- Thorne T, Olson K, Wismer W. A state-of-the-art review of the management and treatment of taste and smell alterations in adult oncology patients. Supportive Care in Cancer. 2015; 23(9): 2843-2851. doi: 10.1007/s00520-015-2827-1.
- Rehwaldt M, Blendowski C, Shott S. Self-Care Strategies to Cope With Taste Changes After Chemotherapy.; 2010.
- de Vries YC, Winkels RM, van den Berg MMGA, et al. Altered food preferences and chemosensory perception during chemotherapy in breast cancer patients: A longitudinal comparison with healthy controls. Food Qual Prefer. 2018; 63: 135-143. doi: 10.1016/j.foodqual.2017.09.003.
- Okuni I, Otsubo Y, Ebihara S. Molecular and neural mechanism of dysphagia due to cancer. Int J Mol Sci. 2021; 22(13). doi: 10.3390/ijms22137033.
- Larsson M, Hedelin B, Athlin E. Lived Experiences of Eating Problems for Patients with Head and Neck Cancer during Radiotherapy. Vol 12.; 2003.
- Kristensen MB, Isenring E, Brown B. Nutrition and swallowing therapy strategies for patients with head and neck cancer. Nutrition. 2020; 69. doi: 10.1016/j.nut.2019.06.028.
- Galaniha LT, Nolden AA. Taste loss in cancer patients: clinicians’ perceptions of educational materials and diagnostic tools. Supportive Care in Cancer. 2023; 31(6): 349. doi: 10.1007/s00520-023-07794-4.
- Milliron BJ, Packel L, Dychtwald D, et al. When Eating Becomes Torturous: Understanding Nutrition-Related Cancer Treatment Side Effects among Individuals with Cancer and Their Caregivers. Nutrients. 2022; 14(2). doi: 10.3390/nu14020356.
- Sevryugin O, Kasvis P, Vigano M, et al. Taste and smell disturbances in cancer patients: a scoping review of available treatments. doi: 10.1007/s00520-020-05609-4/Published.
- Spencer AS, da Silva Dias D, Capelas ML, et al. Managing Severe Dysgeusia and Dysosmia in Lung Cancer Patients: A Systematic Scoping Review. Front Oncol. 2021;11. doi: 10.3389/fonc.2021.774081.
- Rademacher WMH, Aziz Y, Hielema A, et al. Oral adverse effects of drugs: Taste disorders. Oral Dis. 2020; 26(1): 213-223. doi: 10.1111/odi.13199.
- Boltong A, Keast R, Aranda S. Talking about taste how do oncology clinicians discuss and document taste. Cancer Forum. 2011; 35: 81-87.
- Wong HM. Oral complications and management strategies for patients undergoing cancer therapy. The Scientific World Journal. 2014; 2014. doi: 10.1155/2014/581795.
- Epstein JB, Villines D, Epstein GL, et al. Oral examination findings, taste and smell testing during and following head and neck cancer therapy. Supportive Care in Cancer. 2020; 28(9): 4305-4311. doi: 10.1007/s00520-019-05232-y.
- Galaniha LT, Nolden AA. The role of saliva in taste dysfunction among cancer patients: Mechanisms and potential treatment. Oral Oncol. 2022; 133. doi: 10.1016/j.oraloncology.2022.106030.
- Worthington HV, Clarkson JE, Bryan G, et al. Interventions for preventing oral mucositis for patients with cancer receiving treatment. Cochrane Database of Systematic Reviews. 2011; 2021(3). doi: 10.1002/14651858.CD000978.pub5.
- Kapoor, Vikas, Shalini Basur, and Amit Pandey. “Chemotherapy and oral complications-The most neglected side of cancer.” Journal of Advanced Medical and Dental Sciences Research 3, no. 1 (2015): 71.
